Semaglutide (Wegovy®): The weekly shot that causes weight to fall off, but what happens when you stop taking it?
As reported in March of 2021, semaglutide, a diabetes weekly shot, helped nondiabetic overweight and obese adults lose a remarkable amount of weight over a period of 68 weeks.
There were two groups of people, placebo users, and active drug (semaglutide) users. Neither group knew what they were injecting weekly to remove the “placebo effect”.
Both groups were instructed to stick to a lower-calorie diet, about 500-kcal less than usual diet, as well as physical activity of 150 minutes a week (such as walking 30 minutes a day, 5 days a week).
In the first 20 weeks, those injecting placebo drugs lost about 4% of body weight, and those on semaglutide lost about 10% of body weight.
Between 20-68 weeks, the placebo group didn’t change much, in spite of being instructed to eat 500-kcal a day less and exercise 150 minutes a week. While the semaglutide group continued to lose weight to about 17% of body weight at 68 weeks.
Plateau effect:
There seems to be a plateau effect with efforts to lose weight. The reason isn’t clear but seems to be tied into energy intake vs energy expenditure. That would be logical, but something else is at play, and scientists haven’t been able to pin it down in a single, easy to explain, mechanism.
A kilogram of fat contains about 7,700-kcal. So then a pound of fat is about 3,500-kcal. In the semaglutide study, both placebo and treatment groups were supposed to go on a 500-kcal a day restricted diet, in other words, eat 500-kcal less than usual.
If it were linear, that is, calories in vs calories out, the placebo group (if they followed the rules) should have lost 500-kcal a day, or 3,500 a week, or 1 lb of weight a week. Then 20lbs at 20 weeks. This did not happen.
Other studies following the same type of plan, putting people on 500-kcal less eating per day and light exercise, saw about the same thing, 10 lbs in a year vs the 1 lb a week or 52 lbs a year that should occur if it were as simple as calories in and calories out.
Wegovy use wasn’t long enough to know if there is a plateau effect
But weight loss did slow down. Semaglutide is dosed at a very small dosage for the first four weeks and increased every 4 weeks until the final dose of 2.4 mg per week is achieved. So the first 16 weeks are at a lower dosage than the long-term 2.4 mg dose. But in those first 16 weeks, the group taking semaglutide lost about 8% of their body weight. To be in perspective, if one weighed 200 lbs, the loss would be 16 lbs compared to the diet and exercise alone group (placebo). So the drug helped individuals lose almost three times as much weight as diet and exercise alone can.
They stopped the study (the published study, there will be other follow-up studies in the future) at 68 weeks, and leading up to those final weeks the progression of weight loss did appear to slow down but did not clearly plateau. So we don’t know yet.
What happens when the individuals stopped the semaglutide?
In the study, they had a group of semaglutide users stop the drug and stop the lifestyle changes. Now, this seems absurd, to instruct someone who just lost, say 40 lbs, to go back to their old habits. But the drug company was trying to prove a point. Obesity is a chronic condition, and their medication should be taken forever. And they would like Wall Street to know that their customers who lose weight on Wegovy® will have to take it forever (with an average cost of over $1,600 a month) so they can make billions of dollars annually.
Here is what happened: The researchers had a group of the original drug and placebo users stop the lifestyle changes (diet and exercise) and stop the injections until 120 weeks. As a result, the semaglutide users gained weight, but were still 5.6% lighter than the start (so about 11 lbs lighter if they started at 200 lbs). The placebo group, who only did diet and exercise, no real drug, gained essentially all of the weight back.
If this seems ridiculous to you, that a group of researchers developing a weight loss drug would deliberately ask people to gain weight, here is why:
This is how it works with drug companies. They are making a drug, investing millions if not billions of dollars to get it approved and into pharmacies. If the condition that they are treating goes away, it wasn’t worth the dollars of research and development. This only makes sense for them.
But in the original study (where they compared placebo to semaglutide), the placebo group lost weight quickly, most of the weight came off in the first 3 months, and they kept it off for the 14 months of the study. Only when they were told to go back to their old habits at 14 months, did they regain the weight.
What we will never know from this study (because it makes no economic sense for the drug company to sponsor such an experiment) is what would happen if they told both groups to go off the shots, but continue the lifestyle changes. We can assume that the placebo group would have stayed leaner, as they already proved that over about a year, we don’t know how much of the weight would have stayed off of the semaglutide group. It is likely substantial as they did so much better than the placebo group when they went back to their old lifestyle.
Drug therapy without lifestyle intervention for weight loss might be nice, but it probably isn’t cost-effective.
Wegoovy® probably would have led to weight loss, even if the drug company did the study without lifestyle modification. After all, their drug retails for almost $20,000 a year. We don’t currently know what would happen if someone made a serious attempt to lose weight and used semaglutide as a booster to get over the initial hump of initiating a lifestyle change. The drug does make you less hungry and less craving for unhealthy food.
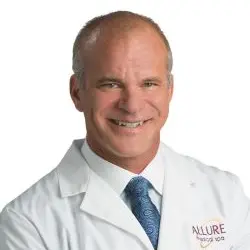
We are trying out the use of semaglutide and different lifestyle intervention in our South Carolina offices of Allure Medical.
The branded drug, Wegovy® is out of stock for the starter dosage, and it isn’t clear if this will be available later in the year. So we are using a compounding pharmacist to source the generic ingredients and prepare them for our staff who want to try them. As a company, we pay for the staff’s lunches, and use a caterer who makes healthier, lower-calorie food than we would eat if we used local fast food establishments.
As a group, the company is paying for 14 weeks of semaglutide with B12 (the vitamin B12 apparently reduces the mild gastrointestinal side effects that can occur with semaglutide) for those who are willing to make a lifestyle effort. And we will see what happens if we discontinue the drug, but maintain the lifestyle changes. They didn’t offer that in the drug company study (that is reported anyway).
Additionally, the compounded semaglutide is far less expensive than the branded version. The 14 weeks will cost about $750 per person (for the entire 14 weeks).
We will update you with the results of this group approach (co-workers) and company-supported (meals and medication) effort to create a healthier community.
Dr Charles Mok
References
Once-Weekly Semaglutide in Adults with Overweight or Obesity. NEJM, March 18, 2021. Vol 384. No 11.Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab 2022 Apr 19.
Wegovy (semaglutide): a new weight loss drug for chronic weight management. Singh G, et al. J Investig Med 2022;70:5–13.
Effect of Intermittent Compared With Continuous Energy Restricted Diet on Glycemic Control in Patients With Type 2 Diabetes: A Randomized Noninferiority TrialJAMA Netw Open 2018 Jul 6;1(3):