How to feel better, look great, lose weight, and reduce your risk of breast cancer and heart disease
This is an overview of the best practice in medicine for dealing with menopause. On prior blog posts, I’ve shared most of the references, so won’t repeat them here unless it’s new information.
Hormone replacement therapy for women entering menopause was pretty much the standard of care in the 1980s, ‘90s and early 2000s. Then the Women’s Health Initiative Trial (WHI) cast doubt on the safety of artificial hormone drugs by reporting there was a slight increased risk of heart disease and breast cancer in women who started on hormone replacement 10 to 15 years after the onset of menopause.
After that study, there was about a 50 percent reduction in hormone replacement prescriptions. But it turns out the initial results of the WHI study were inherently flawed. Instead of a slightly increased risk of heart disease in postmenopausal women when started on synthetic hormone drugs, there was actually a 40 percent reduction in heart attacks for women who started hormone replacement within 10 years of the onset of menopause. Estrogen was actually cardioprotective.
There been other studies since that time, notably the ELITE (Early Versus Late Intervention Trial with Estradiol) study published in 2016, which show us that the cardiovascular protection from estrogen only occurs when started within six to 10 years of the onset of menopause. After then there is no benefit — nor harm.
Multiple studies in the United States and abroad have shown that synthetic hormone drugs are linked to slightly increased risks in breast cancer. These drugs include the horse-based estrogen called Premarin that we use in United States, and another synthetic drug progestin called Provera. However, with the commonly available actual human identical hormones (what people refer to as “natural hormones”) there is no increased risk, and perhaps a slightly reduced risk.
Let’s go a step further.
Hormone Replacement and the Heart
The WHI showed a 40 percent reduction in heart attacks in women who started hormone replacement therapy within 10 years of menopause and continued them long-term. A Danish study using human estrogen (rather than horse estrogen) in addition to synthetic progestin found that not only did hormone replacement lower the rate of heart disease, but the longer women were on it, the more protection they had from heart disease and all causes of mortality. In the 16-year follow-up to this Danish study, woman had about a 50 percent reduction in heart attacks and a more than 70 percent reduction in premature deaths.
What About Breast Cancer?
So the WHI, as well as other studies, showed a slightly increased risk of breast cancer in women taking synthetic hormone drugs, and neutral or slight protection against breast cancer when taking actual hormones.
But there was a missing link. Testosterone is a dominant hormone in a young healthy woman, about five to 20 times more abundant than estrogen.
In 2004, a study was done in Australia adding testosterone pellets to the standard hormone replacement therapy of estrogen and synthetic progestin.
They dosed the testosterone at about 1 mg per pound of body weight. The pellets were inserted under the skin to give long-term release, which is known to have a long-term safety record and give very predictable results. The estrogen chosen was somewhat random; they used both horse synthetic estrogen and human identical estrogen called estradiol.
The average age of the women at the start of the study was about 56. They followed them for six years – and what they found was pretty remarkable. In Australia at that time, it was estimated that about 380/100,000 woman-years would develop breast cancer. A person year is a statistical comparison, so we do say the risk is 380 relatively speaking.
For women on synthetic hormone drugs and testosterone, the breast cancer rate dropped to 283/100,000 woman-years.
With the women not on synthetic progestin, but only estrogen and testosterone, the rate of breast cancer fell even lower to 73/100,000 woman-years. That’s an amazing 80 percent reduction in the expected risk of breast cancer!
Numerous studies have been published since that time in which testosterone at the dose of about 1 mg per pound of body weight was used as a pellet or implant. The implants, which are placed through a small incision in the skin, break down over about three months and are repeated.
There are no adverse events related to testosterone replacement therapy, and it has additional benefits such as improvements to sexuality, skin, fullness of hair, and energy. It also leads to weight loss in overweight women, an average of five pounds in six months.
In 2008, a 10-year study was started by breast cancer researchers, as well as members of the National Institutes of Health, so has one year to go until completion. They are using testosterone alone in most women, only occasionally adding estrogen. They have found that over several years, all symptoms of menopause improved, there were no adverse drug events, and there was a 50 to 75 percent reduction in the rates of breast cancer. The reduction in breast cancer rates were based on how long the women were on testosterone replacement. The longer they were on it, the more protection they had. Again, they used the same dosing, about 1 mg per pound as a testosterone pellet.
The Case for Hormone Replacement Therapy
Hormone replacement therapy has huge implications for both men and women. There has been a significant amount of bias against it in the medical community, the FDA, and various medical societies. There are some who recommend that men and women just experience “normal aging” and not treat hormone deficiency. But that would be as absurd as not treating hypertension, diabetes, heart disease, or cancer.
We’re talking about a treatment that specifically deals with diseases associated with “normal aging.” In both men and women, hormone replacement therapy has been linked to cardiac protection, less cancer, less hypertension, better cardiac lipids, and favorable effects on weight, sexuality, mood, and quality of life.
Just as a side note, in 2016 a study was published on an evaluation of 83,000 men in the Veterans Administration health system who had low testosterone. About half the men with low testosterone were treated with testosterone replacement, and the other half were not treated. Their average age was 66. They were followed for six years.
The men on testosterone replacement had one half the death rate, and one half the amount of heart attacks and strokes. Furthermore, the testosterone replacement therapy had a substantially favorable effect on weight maintenance, potentially reversing diabetes and improving quality of life.
Yet the FDA has still not approved testosterone replacement for men with low testosterone unless they have a specific disease in their brain or testicles, or an extra female chromosome. Here is a 50 percent less chance of dying, more effective than any other drug, and the FDA says it shouldn’t be used except to treat those conditions. It’s absurd but true.
Women entering menopause, or getting symptoms of hormone imbalance, do have an option. While a laboratory evaluation is done, treatment decisions are based more on the clinical findings than the lab results. Typically, woman who are still having periods are put on a testosterone pellet, 1 mg per pound of body weight. They are also started on oral progesterone, the natural human type.
As a woman enters menopause and stops having periods, her estrogen level drops. At this point we add an estrogen pellet comprised of estriol and estradiol. The dose is generally about 10 mg, which is one-tenth the amount of testosterone. This is the natural ratio in your body when you’re much younger.
Women with specific concerns about breast cancer, and at no real risk factor for developing heart disease, may choose to forgo estrogen replacement therapy. Estrogen replacement has been implicated in the development of breast cancer, but it turns out we were just wrong. Yet that does not reduce the bias in the medical community or the public at large.
In that case, a woman can go on just testosterone alone. As studies have shown with more than 1,000 women followed for several years, it works just fine for relieving symptoms of menopause, and reduces the risk of breast cancer by more than 50 percent. There is no evidence that you get as much cardiac protection, but you will get some. Long-term studies following women for up to 16 years show an over 50 percent reduction in heart attacks and premature death when estrogen is added.
In cases where women have been treated for breast cancer, the use of estrogen has been controversial. Studies have shown that the recurrence rate is no higher when estrogen is added, yet there still may be fear and/or bias against its use. In this situation, I use a testosterone pellet along with an estrogen blocker. Again, you’ll get all the benefits of hormone replacement, but likely not as much cardiac protection (although no more risk).
In summary, it is important to understand that you have choices in your health care. In the 1980s and ‘90s, doctors were prescribing hormone replacement routinely for women because we knew it protected their hearts, made them feel better, and improved their quality of life. After the initial WHI results were posted, there was an immediate 50 percent reduction in hormone prescriptions, and this has permanently biased physicians ever since. They haven’t read the updated studies that showed there was actually a 40 percent reduction in heart attacks in women with hormone replacement, and that full hormone replacement, including testosterone, reduced the risk of breast cancer by over 50 percent. As we mentioned, these clinical studies did not make the news the way the original WHI results did — which were flawed.
The importance of spreading the word, of getting doctors to read the clinical studies that been published since the flawed 2002 WHI, is paramount. We have let bias and the misinterpretation of clinical results affect prescribing habits in our nation to the detriment of the health of millions of women.
In my 2017 book, Testosterone, Strong Enough for a Man, Made for a Woman, I detail results of those studies so that you can understand them without being an expert in medical literature, statistics, and clinical data. Please read this book to get a better understanding of something that is of critical importance to your future health.
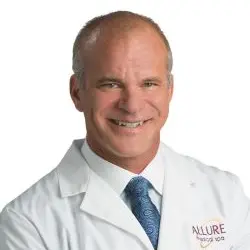
Thank you,
Dr. Charles Mok